The professional coursework is grounded in the mission of the program and university. The curriculum is a blended design with traditional and systems-based approaches. It embeds movement systems within professional practice management themes. Contemporary PT practice with use of the evidence to inform clinical practice is incorporated through a combination of didactic, laboratory, service-learning, and clinical experiences that develop students across the cognitive, affective, and psychomotor learning domains. The curriculum directly reflects the skills, professionalism, leadership, and critical reasoning necessary for entry-level, contemporary physical therapy practice, and life-long learning expected across the span of graduates’ careers.
The framework for the SOPT curriculum plan is built around the following organizational principles, based on SOPT’s philosophy and beliefs:
- Clinical Reasoning
- Leadership
- Professionalism
- Collaboration
- JEDI (justice, equity, diversity, and inclusion)
These principles govern the curriculum model that is built on three pillars that are applied within the integrated and full-time clinical experiences, ultimately leading to SOPT’s expected student/graduate outcomes through a variety of teaching methods and learning experiences:

Movement Sciences including anatomy, physiology, genetics, exercise science, biomechanics, kinesiology, motor control, motor learning, neuroscience, pathology, pharmacology, diagnostic imaging, history, nutrition, and psychosocial aspects of health and disability.
Professional Practice including cardiovascular, endocrine and metabolic, gastrointestinal, genital, reproductive, hematologic, hepatic and biliary, immune, integumentary, lymphatic, musculoskeletal, nervous, respiratory, renal and urological systems, system interactions, differential diagnosis, and the medical and surgical conditions across the lifespan commonly seen in physical therapy practice.
Behavioral Sciences including content and learning experiences in communication, ethics, values, leadership, management, finance, teaching, learning, law, clinical reasoning, evidence-informed practice, and applied statistics.
The curricular model is designed to produce a knowledgeable, reflective generalist who offers evidence-informed, quality care in a compassionate and professional manner as a competent member of the interprofessional team in rural and medically underserved communities. This solid foundation in the signature pedagogy of applied movement science and collaborative practice allows graduates to assume the role of a movement expert, researcher, educator, consultant, administrator, leader, and advocate within the interprofessional health care team.
To reinforce this model and the program’s mission and vision, five transcurricular threads were developed to provide a platform, not only for characteristics sought in students admitted to the program, but also to inform goals for graduates in meeting the needs of society. These are:
Rural and Medically Underserved: Students will provide a continuum of care for rural and underserved communities that is safe, effective and efficient in all aspects of patient management, interpersonal relations, and professional conduct, while demonstrating responsiveness to the individualized needs and well-being of clients/patients “regardless of age, gender, race, nationality, religion, ethnicity, social or economic status, sexual orientation, health condition, or disability”.
Movement Experts: The student will articulate the importance of movement systems across the lifespan through the application of course content to the practice of physical therapy, research, and education to meet the vision of the profession to “transform society by optimizing movement to improve the human experience.”
Interprofessional Practice: Students will develop the core competencies needed for effective collaborative practice.
Evidence-Informed Practice: The student recognizes and demonstrates the ability to critique assigned readings and other published literature taking “personal responsibility for their professional development based upon critical self-assessment and reflection” within the context of the advancement and innovation of physical therapy practice.
Social Justice: The student will demonstrate “respect, the inherent dignity and rights of all individuals” in all aspects of their role as a healthcare provider assuring recognition of their personal biases to prevent discrimination against others while demonstrating independent and objective professional judgment in the patient/client’s best interest within the physical therapists’ scope of practice.
Student/Graduate Outcomes
- Integrate the biological, physical, behavioral, and movement sciences necessary for entry-level physical therapy practice.
- Communicate through words and actions in a professional, compassionate, and ethical manner in all encounters with patients/clients, peers, faculty, families, other professionals, and community/professional leaders.
- Practice in a collaborative manner that is consistent with established legal and professional clinical practice standards.
- Demonstrate sound clinical decision-making skills, including clinical reasoning, clinical judgement, differential diagnosis, reflective practice, and self-reflection/assessment that can be applied in the rural and medically underserved community setting.
- Apply existing research to inform clinical decision-making skills and innovative physical therapist practice based on solid theoretical constructs.
- Lead to advocate in communities and the physical therapy profession.

Download single page plan of study
COURSE DESCRIPTIONS
Year 1
FALL SEMESTER
PHTH 500 Foundations of Clinical Practice I (3.5 cr hrs) The first in a series of three courses focused on clinical skills and patient management processes in the physical therapy setting. Foundational knowledge and skills related to the medical interview, motivational interviewing, basic examination procedures are developed and form the basis for systems-based patient management throughout the curriculum. Laboratory sessions focus on foundational psychomotor skills including, but not limited to infection control, body mechanics, safety, proper draping, vital signs, palpation, neuromuscular screen, the application of goniometry for assessment of range of motion, manual muscle testing, and anthropometric measures. The inclusion of defensible documentation utilizing the patient/client management model with appropriate medical terminology reflects the International Classification of Function framework. A combination of lecture, laboratory, small group, case-based learning, with use of standardized patients (SPs) will enhance student learning. Formative assessment experiences in the form of clinical communication such as SBAR (situation, background, assessment, recommendation) and the communication assessment tool are reinforced. (2 hr lect/3 hr lab)
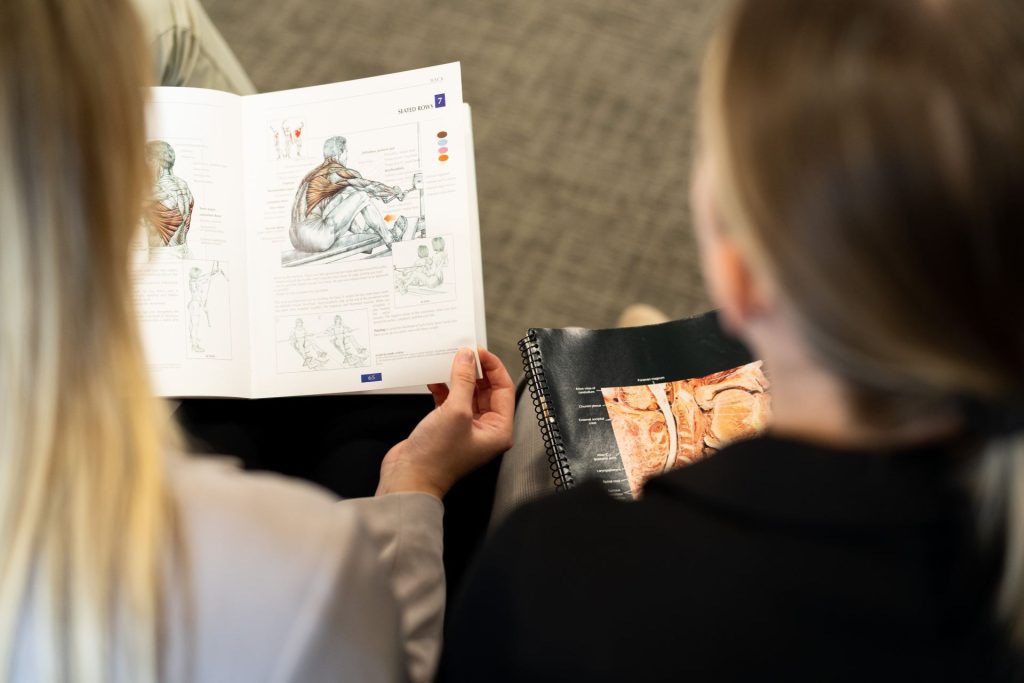
PHTH 505 Gross Anatomy (4.5 cr hrs) This lecture and dissection/pro-section-based course integrates Doctoral Physical Therapy and Osteopathic Medicine students. The content is divided into four units, based on regional anatomy: back, upper limb, lower limb, and thorax. Lectures on fundamental radiological anatomy related to the area under study occurs near the end of each unit. Basic neuroanatomy is integrated throughout the course as a precursor to PHTH 506 Applied Neuroscience. This course provides the student with a solid knowledge base in gross, neurologic, and radiologic anatomy. The regional anatomic presentations are essential for preparing healthcare professions to integrate patient presentation for application of clinical differential diagnosis and treatment imperative as an effective doctoral physical therapist practitioner. (2 hr lect/4 hr lab)
PHTH 510 Lifespan Development (2 cr hrs) Normal and abnormal human embryonic development will set the stage for the mechanisms of and clinical relevance for the establishment of normal development of: gross motor, fine motor, language, cognition, psychosocial, and play skills across the lifespan. The foundation of movement analysis is established through the context of neuromotor control development which underlie skilled performance in everyday functional behaviors from infancy through older age. Applied relevance of current perspectives in motor control and learning will be addressed through application of current principles to understand optimal movement development across the lifespan. Students will be exposed to live examples to integrate age related development across the lifespan. (2 hr lect)
PHTH 512 Movement Science I (3 cr hrs). Principles, theories, and applications of static and dynamic biomechanics are presented as it applies to human movement and the study of specific structures involved in the achievement of movement. Emphasis is on the integration of theory, ergonomics, structured movement analysis of activities of daily living, through the application of the International Classification of Functioning, Disability and Health (ICF) model informs clinical decision making within physical therapy practice. The normal gait cycle phases will be emphasized including gait kinetics. Laboratory sessions will include observation and analysis of human movement and function; outcome measures that define the function of movement and application to clinical practice will be explored. Introductory material related to basic mobility and components of normal gait will be presented to reinforce principles of dynamic analysis. (2 hr lect/2 hr lab)
PHTH 515 Intro to Pathophysiology (1 cr hr) The foundation of basic histology and cell function will be used to promote the study of pathophysiology’s disruption of homeostasis and the discerned impact on movement systems, the cornerstone of physical therapy practice. In the first course of the pathophysiology sequence, students will understand the role of physical therapy in screening to assist in the differentiation of pathological etiologies underlying disease and injury. The course introduces the definition of various musculoskeletal and immune system diseases/conditions. Emphasis will be on the incidence, etiology, pathogenesis, and clinical manifestations necessary to identify critical information related to “red flags” that may contraindicate physical therapy treatment and/or indicate referral to another health care professional. Medical, surgical, and rehabilitation management of specific conditions are also explored. (1 hr lect)
PHTH 520 Professional and Interprofessional Practice I (2 cr hrs) The first in a series of three courses that integrates diverse interprofessional perspectives to prepare students for effective practice as collaborative team members. The Interprofessional Education Collaborative (IPEC) core competencies will be reinforced to foster team-based and patient-centered practice. This course addresses professional behavior standards in relation to patient care interaction and collegial relationships including roles and responsibilities in relation to physical therapist assistants. The preparation of students to manage professional and ethical responsibilities of the physical therapy practice in the delivery of health care services such as application of core values, the physical therapist practice act, and APTA code of ethics. TeamSTEPPs training will be used to inform students of techniques and strategies to improve patient safety and interprofessional communication. This course incorporates cultural competency for addressing diversity, patient learning styles, patient education, patient health behavior models, conflict resolution, and issues of professional advocacy are also addressed. (2 hr lect)
PHTH 545 Evidence Informed Practice (3 cr hrs) Application of the principles of evidence-informed practice to inform clinical decision making. Students will become proficient with application of PICOTS (patient problem, intervention, comparison, outcome, time, setting) strategy for literature search, application of the methods of scientific inquiry including AMA formatting, research theory, design, methods, and measurement. Statistical analysis will assist students with the ability to draw research conclusions, assure the validity of research evidence for clinical practice application and learn specific statistical tests utilized for descriptive and inferential analysis of experimental research data. Understanding of research design, methods, and statistical assessment will be captured through a critical analysis of the literature (CAT) assignment to inform the process for the application of a systematic review of the literature as a precursor for the capstone project. (3 hr lect)
SPRING SEMESTER
PHTH 501 Foundations of Clinical Practice II (3.5 cr hrs) This course is a continuation of PHTH 500 with further application of physical therapy examination, evaluation, and treatment skills commonly used in physical therapy practice. Instruction will include, the integumentary screen, application of personal protective equipment, advanced transfer techniques, functional balance testing, basic heat/cold interventions including ultrasound. Additionally, students will be introduced to components and prescriptions of therapeutic exercise and movement-based intervention. A combination of lecture, laboratory, small group, case-based learning, with reinforcement and practice of learned skills through the use of the standardized patient (SP) will enhance student learning. Students will encounter acute and chronic problems in diverse patient centered cases and apply their movement science knowledge to promote readiness for clinical education. Concepts of empathic communication and cultural humility will be reinforced. (2 hr lect/3 hr lab)
PHTH 506 Applied Neuroscience (3.5 cr hrs) Advanced study of structures, organization, and function of the nervous system with emphasis on the neuroanatomical structures and neurophysiological functions of the motor and sensory systems that regulate movement. Understanding clinical manifestations seen in various neurological diseases is the foundation for evaluating and treating patients with neurological disorders. Human brain specimens will supplement lecture material. Other lab activities emphasize elements of the neurologic examination and apply common outcome measures and assessment tools. Clinical skills will be reinforced and practiced with volunteers with various neurological diagnoses from the community. Neuroradiology, focusing on the central and peripheral nervous system, spine, head, and neck using neuroimaging examples are also presented. (2 hr lect/3 hr lab)
PHTH 513 Movement Science II (3 cr hrs) Advanced study of normal and abnormal gait, principles of ergonomics, biomechanics of posture and interpretation of functional capacity evaluations. Students will learn to assess normal and abnormal gait of selected pathologies that commonly present in physical therapy practice. Conditions and impairments requiring lower quarter orthotic and prosthetic intervention will be presented, including pre/post op care, examination/evaluation, device design and prescription, proper device fitting and training. Outcome measures commonly administered in patients with gait deficits will be highlighted. Lab activities emphasize advance analysis of pathological movement through motion analysis technology, and rehabilitation interventions for individuals utilizing orthotics or prosthetics for functional mobility. (2 hr lect/2 hr lab)
PHTH 514 Exercise Physiology (2 cr hrs) Systems approach to the body’s response and adaptation to exercise training interventions within physical therapy practice. Students will interpret the influence of static and dynamic factors of physical activity within the context of acute response and chronic physiologic adaptations based upon intensity, frequency and duration of exercises and rest. The prescription of exercise for specific populations are emphasized. The effects of nutrition and exercise across the lifespan are also highlighted. (2 hr lect)
PHTH 516 Applied Pathophysiology (3 cr hrs) The second course of the pathophysiology sequence will build upon the foundations taught in PHTH 515. Students will discern the impact of pathophysiologic conditions related to the following systems: cardiovascular, pulmonary, lymphatic, endocrine, gastrointestinal, renal, urogenital, hematologic, neurological, integumentary, and reproductive. Various diseases and their incidence, etiology, pathogenesis, and clinical manifestations will continue to be covered specific to each system. Discussions will include genetic factors and their influence on risk, progression, outcomes, and response to rehabilitation interventions. Medical, surgical, and rehabilitation management of specific conditions is also explored. (3 hr lect)
PHTH 521 Professional and Interprofessional Practice II (2 cr hrs) The second in a series of three courses that will integrate diverse interprofessional perspective to prepare students for effective practice as collaborative team members. Topics relative to healthcare delivery models will focus on the healthcare system in the United States, rural, and community health. The course reviews community health services, prevention, wellness, health policy, reimbursement, fraud, and the professions obligation as a mandated reporter. Advocacy will be addressed through the WA State Legislative Impact Day. (2 hr lect)
PHTH 543 Integrated Rural Clinical Outreach I (1.5 cr hrs) This experiential service-learning course is designed to engage students in analyzing healthcare access through a community needs assessment, health literacy instruction, social determinates of health, and interprofessional clinical practice in rural and medically underserved areas. Students will develop an understanding of the demographics, economics, and structure of the rural healthcare delivery system in America, with a concentration to the diverse population found in the Northwest. Additionally, current Federal and state health policy will be examined with special attention on reports from the Center for Rural Affairs and reform legislation addressed by the U.S. Congress and the White House. Primary, secondary, and tertiary care models will be discussed with emphasis on medical screening, referrals, interprofessional collaborative practice, and physical therapist scope of practice. Students will work under the direction of licensed physical therapy faculty at various community rural health care facilities. (0.5 hr lect/2 hr lab/clinic)
PHTH 550 Clinical Competence in Patient Management I (0.5 cr hr) Clinical laboratory simulation methods will be used to assess students’ ability to formulate a plan of care based on the patient/client management model. Students’ knowledge, clinical reasoning, and clinical practice skills will be assessed utilizing a simulated Standardized Patient emphasizing the first year of coursework. The student must pass this exam to enroll in PHTH 600 Clinical Experience 1 (CR/NC) (1 hr lab)
Year 2
SUMMER SEMESTER
PHTH 600 Clinical Experience I (4.5 cr hrs) This nine-week full-time clinical experience during summer semester following completion of Year 1 allows the student to apply didactic knowledge, foundational professional clinic skills, clinical reasoning, as well as incorporate and refine cognitive, affective, and psychomotor skills in a clinical setting. Comprehensive examination, evaluation, and intervention will be used to manage the physical therapy patient. By the end of the clinical experience, students are expected to demonstrate advanced beginner to intermediate performance levels on the Physical Therapist Clinical Performance Instrument Web (PT CPI). CR/NC grading only.
FALL SEMESTER
PHTH 607 Neurological Movement System I (4.5 cr hrs) Management of individuals with neurologic health conditions, with emphasis on acquired brain injury including stroke/cardiovascular accident, Parkinson’s, other balance and vestibular disorders, based on neurophysiological and pathokinesiological mechanisms that result in movement system impairments in body structure/function, activity limitations, and participation restrictions. A focus on the development of advanced knowledge and application of skill during patient/client screening, examination, evaluation, outcome measures appropriate for this population, development of a comprehensive plan of care, and clinical decision making using the best evidence for application of treatment procedures across the continuum of care. Correlation of deficits in these neuro populations will be completed with advance diagnostic imaging examples. Emphasizes the application and integration of motor control/learning, theoretical constructs, evidence-informed practice, and the patient/client management model.
(3 hr lect/3 hr lab)
PHTH 620 Musculoskeletal Movement System I (4.5 cr hrs) The first in a series of two courses building on first-year content within the movement sciences. Analysis of musculoskeletal movement system impairments in body structure/function, activity limitations, and participation restrictions of the extremities will be highlighted. Emphasis on physical assessment, interpretation/evaluating of examination findings including outcome measures, application of therapeutic intervention methods such as joint mobilization/manipulation, soft tissue mobilization, therapeutic exercise, with focus on clinical decision making, and establishment of the physical therapy plan of care. Students will conduct a search of the literature and apply evidence to facilitate the application of current relevant clinical knowledge to clinical cases. Selected lectures by medical practitioners will enhance student knowledge of imaging and medical-surgical management of orthopedic conditions. (3 hr lect/3 hr lab)
PHTH 622 Professional and Interprofessional Practice III (2 cr hrs) The final course in a series of three courses that integrates diverse interprofessional perspective to prepare students for effective practice as collaborative team members. This course presents topics relative to health disparities especially for the rural population, health status indicators, health policy, social determinants of health, cultural competency, ethical dilemma resolution including a simulated abuse case utilizing the Realm-Individual Process-Situation (RIPS) model of ethical decision making, global health, and access to health services. This course will also encompass in-depth perspective of compassionate care as it relates to cultural competencies, therapeutic alliance, patient education and rights, including issues of death and dying. (2 hr lect)
PHTH 625 Cardiopulmonary Movement System (3.5 cr hrs) Clinical assessment and management of patients with movement-related cardiovascular and/or pulmonary conditions. A focus on the development of advanced knowledge and application of skill during patient/client screening, examination, evaluation, outcome measures appropriate for this population, development of a comprehensive plan of care, and clinical decision making using the best evidence for application of treatment procedures across the continuum of care. EKG interpretation, understanding impact of stress testing, heart and lung auscultation, pulmonary function testing, principles of cardiac rehabilitation, lines and lead management, respiratory airway clearance techniques/chest physical therapy will be integrated during lab activities. Treatment techniques will include patient education including nutrition, administration and dosing of therapeutic exercise and conditioning, breathing techniques, airway clearance, percussion and postural drainage, medical and surgical management, and the potential for recovery for selected acute and chronic conditions across the lifespan. Interpretation of laboratory tests, imaging, and pharmacology will prepare students to safely work with high acuity patients. Nutrition education within the physical therapist’s scope of practice will help to promote a healthy lifestyle for those living with cardiac and pulmonary disease. Case studies, simulated standardized patients, and high-fidelity manikin simulation in a multidisciplinary approach will provide students with real-world exposure to acute and critical care scenarios. Students will conduct a search of the literature and apply evidence to facilitate application of current relevant clinical knowledge to clinical cases. (2 hr lect/3 hr lab)
PHTH 635 Clinical Reasoning I (2 cr hrs) Builds on early skills developed in the first-year courses leading to the ability to make informed clinical decisions. Problem-based and case-based learning activities will be incorporated with simulated standardized patients to further develop critical thinking and reasoning skills for the establishment of the physical therapy diagnosis and plan of care which incorporates the International Classification of Functioning, Disability and Health (ICF) model. Also, current teaching and learning methods will be discussed to improve the student’s ability to educate their patients. The curriculum will include introduction to telehealth history, regulation, reimbursement, and HIPAA protection. Students will conduct a search of the literature and apply evidence to facilitate application of current relevant clinical knowledge to clinical cases. Additionally, as part of this course, students will present a complex patient case from their summer full-time clinical experience with emphasis on applying the Guide to Physical Therapy Practice as a framework for clinical decision-making skills. (2 hr lect)
PHTH 644 Integrated Clinical Practice I (1.5 cr hrs) This experiential service-learning course is the first of two courses designed to progress the development of clinical competencies needed of an independent physical therapy practitioner in the outpatient setting. Under faculty mentoring, student physical therapists will practice clinical decision analysis and clinical skills in a community-based teaching research lab, the Center for Applied Movement Science (CAMS), at PNWU. This course is designed to allow the student physical therapist to apply and integrate academic knowledge of the examination, evaluation, outcome measures appropriate to this population, diagnosis, prognosis, and management of participants with a neurologic, gait, or balance deficit in a clinical setting. Emphasis on patient/clients with balance and movement disorders from acquired brain injury (CVA), Parkinson’s disease, or vestibular impairments. Instruction includes essential and assistive technology competencies that improve function or help manage healthcare delivery in a constantly changing digital world. Software and mobile apps are leveraged to improve communication, facilitate learning, and enhance clinical practice and patient outcomes. A patient-centered approach to health and disease is presented to help students recognize conditions both at risk for advanced chronicity and outside the scope of physical therapy.
(0.5 hr lect/2 hr lab/clinic)
PHTH 646 Capstone I (1 cr hr) The first in a series of three courses introduces the capstone project, (case study, evidence-based project, or clinical research) reinforcing the concept of the physical therapist as researcher and scholar, representing the culmination of the doctor of physical therapy degree. This venue provides an opportunity for the student to demonstrate independence in critical thinking, appraisal of research literature, the ability to compile and organize information for disseminating evidence-informed material on a topic related to physical therapy. In this preliminary course, students will complete a search of the literature in order to complete a draft of the introduction, review of the literature, as well as explore and identify potential research statistic methods for their project. Students are assigned a faculty mentor to assist in the exploration and development of their Capstone project. CR/NC grading only.
(2 hr/wk independent study)
SPRING SEMESTER
PHTH 602 Foundations of Clinical Practice III (3.5 cr hrs) Continuation of PHTH 500 and PHTH 501 with further application of physical therapy examination, evaluation, and treatment skills commonly used in clinical practice. Advanced theories and principles will be presented related to pain science, treatment of chronic pain, tissue healing, electrophysiological modalities and electro-neuromuscular stimulation for motor performance, nerve function, pain management and tissue repair. Critical appraisal of current evidence examines the physical and physiological effects of these modalities, with emphasis on pain, inflammation, tissue healing, and muscle reeducation. Clinical decision-making emphasizes the appropriate selection of physical agents and treatment parameters based on patient indications and contraindications/precautions with focus on desired treatment effects. Laboratory sessions develop skills for the safe and effective clinical application of physical agents and therapeutic modalities. A combination of lecture, laboratory, small group, case-based learning, and standardized patients (SP) will enhance student learning. Formative assessment experiences with standardized patient encounters, and reflections will further assist integration and application of concepts presented in the course. (2 hr lect/3 hr lab)
PHTH 608 Neurological Movement System II (3.5 cr hrs) Management of individuals with neurologic health conditions, with emphasis on traumatic brain injury, spinal cord injury, Guillain Barre syndrome, amyotrophic lateral sclerosis, and multiple sclerosis based on neurophysiological and pathokinesiological mechanisms that result in movement system impairments in body structure/function, activity limitations, and participation restrictions. A focus on the development of advanced knowledge and application of skill during patient/client screening, interpretation of advanced diagnostic modalities/imaging, examination, evaluation, outcome measures appropriate for this population development of a comprehensive plan of care, and clinical decision making using the best evidence for application of treatment procedures across the continuum of care. Correlation of deficits in these neuro populations will be completed with advance diagnostic imaging examples. Emphasizes the application and integration of motor control/learning, theoretical constructs, evidence-informed practice, and the patient/client management model. (2 hr lect/3 hr lab)
PHTH 621 Musculoskeletal Movement System II (5 cr hrs) Continuation of PHTH 620 with focus on movement system impairments involving the spine, TMJ, core, and pelvic girdle. Analysis of musculoskeletal movement system impairments in body structure/function, activity limitations, and participation restrictions. Emphasis on physical assessment, interpretation/evaluating of examination findings including outcome measures, application of therapeutic intervention methods such as joint mobilization/manipulation, soft tissue mobilization, therapeutic exercise, with focus on clinical decision making, and establishment of the physical therapy plan of care. Students will conduct a search of the literature and apply evidence to facilitate application of current relevant clinical knowledge to clinical cases. Selected lectures by medical practitioners will enhance student knowledge of imaging and medical surgical management of orthopedic conditions. (3 hr lect/4 hr lab)
PHTH 626 Management of Select Populations I (2 cr hrs) Clinical assessment and evaluation of patients with integumentary and lymphatic pathology sets the stage for this course. Normal tissue anatomy, wound healing, nutrition, vascularization, and factors that adversely affect healing are discussed as a foundation for wound management. Examination, evaluation, diagnosis, prognosis, interventions and outcomes for persons with various types of wounds will be covered using video demonstration and clinical cases. Specific integumentary disorders are discussed including arterial and venous insufficiency ulcers, pressure ulcers, neuropathic ulcers, lymphedema, and burns. Application of specific tests and measures, their reliability and validity, and efficacy of and skill development for treatment interventions such as pulsed lavage, sharp debridement, wound vac application will be covered. Lymphatic circulation and stages of lymphedema will be addressed in preparation for the second in the series addressing treatment of the lymphatic system. A focus on the development of advanced knowledge and application of skill during patient/client examinations, evaluation, development of a comprehensive plan of care, and clinical-decision making using the best evidence for application of treatment procedures in the treatment of the integumentary system. (1 hr lect/2 hr lab)
PHTH 645 Integrated Clinical Practice II (1.5 cr hrs) This experiential, service-learning course is the second of two courses designed to progress the development of clinical competencies needed of an independent physical therapy practitioner in the outpatient setting. Under faculty mentoring, student physical therapists will practice clinical decision analysis and clinical skills in a community-based teaching research lab, the Center for Applied Movement Science (CAMS), at PNWU. This course is designed to allow the student physical therapist to apply and integrate academic knowledge to the examination, evaluation, outcome measures appropriate to this population, diagnosis, prognosis, and management of participants with a neurologic, gait or balance deficit in a clinical setting. Emphasis on patient/clients with balance and movement disorders from peripheral nerve injury such as spinal stenosis, spinal cord injury, traumatic brain injury, concussion, ALS, and multiple sclerosis. Instruction includes essential and assistive technology competencies that improve function or help manage healthcare delivery in a constantly changing digital world. Software and mobile apps are leveraged to improve communication, facilitate learning, and enhance clinical practice and patient outcomes. A patient-centered approach to health and disease is presented to help students recognize conditions both at risk for advanced chronicity and outside the scope of physical therapy. (0.5 hr lect/2 hr lab/clinic)
PHTH 647 Capstone II (2.5 cr hrs) In the continuation of the capstone project series this course will continue to refine student use of the literature and facilitate graduate level writing. Students will develop and submit an abstract for dissemination of their initial research work through presenting the project at the universities research symposium held each April. Students will submit their completed literature review, methods, and initial results (as available) for their project under the guidance of their faculty capstone mentor. CR/NC grading only. (5 hr/wk independent study)
PHTH 650 Clinical Competence in Patient Management II (1 cr hr) Simulated standardized patient encounters will be utilized to assess students’ ability to formulate a plan of care based on the patient/client management model. Students’ knowledge, clinical reasoning, and clinical practice skills will be assessed utilizing a simulated standardized patient emphasizing the first two years of coursework. The student must pass this exam to enroll in PHTH 700 Clinical Experience II. (2 hr lab)
Year 3
SUMMER SEMESTER
PHTH 700 Clinical Experience II (4.5 cr hrs) This 9-week full-time clinical experience during summer semester following completion of Year 2 allows the student to apply academic knowledge in a clinical setting. Comprehensive examination, evaluation, and intervention will be used to manage the physical therapy patient. By the end of the clinical experience, students are expected to demonstrate intermediate to advanced intermediate performance levels on the Physical Therapist Clinical Performance Instrument Web (PT CPI). CR/NC grading only
FALL SEMESTER
PHTH 709 Pediatric Physical Therapy (3.5 cr hrs) Advanced study of diagnoses and physical therapy management of infants and children with musculoskeletal, neurological, and/or cardiopulmonary impairments. A framework of normal development and aging from birth to young adult is presented and serves as a course foundation. Students will apply motor learning principles to the elements of patient/client management in physical therapy practice, including screening, examination, appropriate outcome measures for the population, evaluation, diagnosis, prognosis, plan of care, intervention, and outcomes related to the pediatric patient. Pediatric imaging examples will be presented. The importance of nutrition, exercise, activities to prevent childhood obesity will be discussed. Students will conduct a search of the literature and apply evidence to facilitate application of current relevant clinical knowledge to clinical cases. Topics include but are not limited to developmental delay and disability, family-centered care, legislation related to provision of pediatric physical therapy services, orthotics, prosthetics, and assistive technologies. (2 hr lect/3 hr lab)
PHTH 722 Geriatric Physical Therapy (3 cr hrs) Synthesis of the biology of aging with common orthopedic and neurologic problems special to the older adult patient. Students will learn key concepts related to the normal aging process versus senescence, age-related disorders, multimorbidity, physical resilience, and pharmacological principles including polypharmacy. This course emphasizes analysis of clinical problems and issues facing the physical therapist in utilizing functional testing and community resources with the elderly. Students will conduct a search of the literature and apply evidence to facilitate application of current relevant clinical knowledge to clinical cases. Students will assess older adults from the community, using age-appropriate assessments to provide recommendations to enhance or facilitate continuance of physical function, independence, and quality of life. (2 hr lect/2 hr lab)
PHTH 723 Administration and Leadership (2 cr hrs) Study of the management of physical therapy practice and leadership development. This course presents an in-depth discussion of administrative issues overarching physical therapy practice, including economic trends, operational policy, budgeting, reimbursement, staffing, business structure, performance improvement, public relations, employment law, quality improvement, and entrepreneurship. In addition, this course will discuss such topics as leadership styles, effective team leadership techniques, application of compliance and motivation principles, peer teaching, consultation skills, decision-making strategies for conflict resolution, and communicating to improve outcomes as a framework for students to develop skills for leadership in daily practice. Students will prepare résumés and begin career planning. (2 hr lect)
PHTH 727 Management of Select Populations II (2 cr hrs) This course examines physical therapy assessment and intervention of specialty diagnosis including cancer, lymphedema, and pelvic/reproductive dysfunction. Cancer components include screening, understanding medical staging and treatment modalities, pharmacology, imaging, and the physical therapist role in facilitating safe and effective movement and exercise in this population. Pelvic health content will include entry level assessment and treatment of sexual dysfunction, incontinence, pelvic floor laxity, pelvic pain, and pregnancy musculoskeletal dysfunction. Lymphedema assessment and treatment including entry level manual decongestive therapies and compression wrapping. Students will conduct a search of the literature and apply evidence to facilitate application of current relevant clinical knowledge to clinical cases. (1 hr lect/2 hr lab)
PHTH 736 Clinical Reasoning II (3 cr hrs) This is the second course in a two-course series which further builds on the ability to make informed clinical decisions. Emphasis on developing an independent practitioner of physical therapy that has the knowledge base and clinical decision-making skills to effectively screen the patient for medical referral and if referral is indicated provide effective communication for transition. Focus is on integrating all parts of patient/client management-examination, evaluation, diagnosis, prognosis, and intervention with emphasis in the practice of screening for medical referral and being able to predict realistic levels of improvement in patients with complex clinical presentations, atypical signs and symptoms, and/or comorbidities. This course will prepare the student to recognize serious pathology, interpret test results, generate a diagnosis, refer to other practitioners, and recognize the indications for physical therapy interventions. (3 hr lect)
PHTH 746 Integrated Rural Clinical Outreach II (3 cr hrs) Experiential service-learning (SL) course designed to challenge the student to manage medically underserved patients/clients in a rural setting with limited resources as an interdependent practitioner working within a collaborative medical model. Additionally, students will gain an understanding of necessary assessments which promotes direct access for health and wellness intervention. Students will be assigned to a community-based health center or clinic under the direction of a faculty member who is a licensed physical therapist. In consultation with faculty clinical instructors and health center staff students are responsible for examination, tests/measures, evaluation, differential diagnosis and development of a plan of care that includes progressive interventions, coordination of care, and patient education for patients. As part of this course, students will also explore the role of physical therapists in the prevention and in the promotion of health, wellness, and fitness. Students will apply this knowledge through the design and implementation of a community-based wellness/prevention program or health fair event that explores health and wellness across the lifespan in selected community agencies in the Yakima Valley.
(1 hr lect/4 hr lab/clinic/SL)
PHTH 748 Capstone III (1.5 cr hrs) This course is the culmination of the Capstone series. Students will finalize their project through the construction of three products, a PowerPoint for their oral defense, a poster for dissemination at the DPT Capstone Symposium, and submission of their final manuscript. The dissemination of their work will be critiqued by their peers, community members, and the profession through the invitation of local physical therapist clinicians. Additionally, students will present an oral defense of their Capstone Project to their Doctoral Committee for final confirmation. CR/NC grading only. (3 hr/wk independent study)
PHTH 750 Clinical Competence in Patient Management III (1 cr hr) Simulated standardized patient encounters will be used to assess students’ ability to formulate a plan of care based on the patient/client management model. Students’ knowledge, clinical reasoning, and clinical practice skills will be assessed utilizing a simulated standardized patient emphasizing the entire curricular model. The student must pass this exam to enroll in PHTH 790 16-week Clinical Experience III in the spring semester. (2 hr lab)
SPRING SEMESTER
PHTH 790 Clinical Experience III (8 cr hrs) This 16-week (or two-8 week) full-time, terminal clinical experience(s) during spring semester of the final year allows the student to apply academic knowledge in a clinical setting. Upon completion of this course, the student must demonstrate mastery of physical therapy skills considered appropriate for entry-level practice on the Physical Therapist Clinical Performance Instrument Web (PT CPI). CR/NC grading only
Doctor of Physical Therapy Program
Mission and Vision
Accreditation
Curriculum Plan
Clinical Education Experiences
Admissions Requirement
Cost of Attendance
Academic Calendar
Information Sessions
Faculty and Staff
Know the PT Field
Student Financial Facts
SOPT Newsletter
Contact Information
Peggy R. Trueblood, PT, PhD
School of Physical Therapy
Professor and Program Director
509.249.7709
ptrueblood@pnwu.edu

For general questions about the DPT program, please email dpt@pnwu.edu or call 509.249.7725.